CHPs Contribute to Abdominal Aortic Anurrysm (AAA) Research)
Abdominal Aortic Aneurysm (AAA) is a life-threatening condition characterized by the extensive remodeling and breakdown of the extracellular matrix (ECM). Understanding the factors governing aortic instability - particularly the micro/nanoscale changes - is paramount for improving AAA management.
A new publication, "Nano-mechanical Mapping of Human and Porcine Abdominal Aortic Aneurysm" uses advanced imaging techniques including atomic force microscopy (AFM) and histology to better understand the nanoscale mechanical heterogeneity in AAA and attempt to attribute its cause
The study utilized AFM to analyze human AAA tissue and a porcine AAA model, generating topographical images and performing Quantitative Nanomechanical Mapping (PF-QNM) to ascertain the local elastic modulus. AFM analysis confirmed that AAA tissue is mechanically heterogeneous, with key findings at the nanoscale. The modulus of collagenous regions was found to be over twice as high as that of non-collagenous (collagen-poor) regions in human AAA tissue.

This highlights the significant difference in stiffness imparted by the collagen-rich structure. Furthermore, both collagenous and non-collagenous regions were interspersed with nanoscale particles exhibiting a significantly higher modulus (5–10 MPa). These stiff locales, postulated to be calcific deposits, had a modulus about three times higher than the surrounding collagenous regions.
How do CHPs contribute?
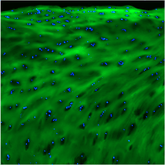
To confirm the presence of calcific deposits and understand their spatial relationship with collagen degradation, the researchers employed a dual histological staining approach. This is where the Collagen Hybridizing Peptide (CHP) played a key role. Tissue sections were dual-stained with Von Kossa (VK), which localizes calcific deposits, and the Collagen Hybridizing Peptide (R-CHP Cy3 Conjugate, 3Helix), which specifically recognizes degraded collagen. By performing this dual-staining , the results demonstrated that calcific deposits (VK-positive) were present in both CHP-positive (degraded collagen) and CHP-negative regions of the AAA tissue.

This suggests that calcification is not restricted to areas of intact ECM but also occurs in regions with degraded collagen, as well as on other ECM components like elastin or proteoglycans. Transmission electron microscopy (TEM) further corroborated this, revealing electron-dense (calcific) deposits on abnormal collagen fibrils and in non-collagenous regions. This led the authors to show that abnormal collagen fibrils can serve as locales for calcific deposits.
By combining cutting-edge AFM nanomechanical mapping with the precision of Collagen Hybridizing Peptide staining, this study has provided crucial insights into the altered nanoscale structure and mechanics in AAA. The results underscore that the mechanical heterogeneity of AAA tissue is driven by the stark difference between collagenous and non-collagenous regions, and the presence of stiff nanoscale calcific deposits, which are often co-localized with areas of degraded or abnormal collagen. These findings improve our understanding of the altered structure and mechanics in AAA and can broadly be applied to the understanding of ECM remodeling and calcification in other vascular diseases.
FULL PAPER:
Pan, Aratrika, et al. "Nano-mechanical mapping of human and porcine abdominal aortic aneurysm." Journal of the Mechanical Behavior of Biomedical Materials (2025): 107229.