Targeted Drug Delivery in Rheumatoid Arthritis: Leveraging Collagen Hybridizing Peptides for Enhanced Therapeutic Efficacy
04 Nov 2024
0 Comments
Histological staining of mouse tibia-talus joints showing healthier articular cartilage due to iFab-CHP treatment compared PBS placebo.
Rheumatoid arthritis (RA) is a chronic autoimmune disease which leads to the breakdown of the cartilage in the synovial joints. Current treatment strategies with tumor necrosis factor-alpha (TNFa) targeting neutralizing antibodies effectively reduce inflammation in the joint space, but also produce undesirable off-target outcomes such as opportunistic infections, congestive heart failure, and pancytopenia. These side effects limit tolerability of these drugs leading to premature termination of treatment and insufficient relief from RA.
Leveraging the fact that damaged collagen is a hallmark of RA pathology, this research group engineered antibody-collagen hybridizing peptide conjugates as a means to target anti-TNFa antibody therapeutics to sites of damaged collagen. They achieved this by covalently attaching the TNFa targeting antigen binding fragment (iFab) from the established RA drug Infliximab with a collagen hybridizing peptide (CHP).
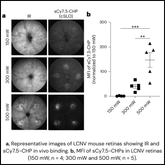
In this study, researchers confirmed successful conjugation of CHP to anti-TNFa iFab as well as retention of collagen and TNFa-binding functions in vitro. They also confirmed retention of homing capabilities in vivo. Upon systemic injection of iFab-CHPs in the tail vein, they saw sustained retention of iFab-CHPs in the spine, ribs, and joints of healthy nude mice with low levels of collagen damage. Since the extent of collagen damage and tissue permeability is much greater in joints is much greater in RA compared to healthy mice, this experiment was useful as a proof of concept for effective drug delivery of iFab-CHP conjugates in vivo.
To verify therapeutic efficacy in vivo, they treated a genetically modified mouse model of RA with iFab-CHP versus a PBS placebo. In this model which over-expressed human TNFa, they observed lower synovial hyperplasia, no evidence of inflammatory cell infiltration, and healthy cartilage by Safranin O staining.
Altogether these results highlight the impressive utility of CHPs as a drug delivery platform in RA, and provide a framework for targeted drug delivery for neutralizing antibodies for other diseases hallmarked by damaged collagen.
Arlotta et. al. Bioconjug Chem. 2020 August 19; 31(8): 1960–1970. doi:10.1021/acs.bioconjchem.0c00324
FULL ARTICLE
Tags: