Shedding Light on Cardiac Repair: How Red-Light Preconditioning Improves Cell Therapy
Following a heart attack, fibrosis is the primary obstacle to recovery. Healthy heart muscle is replaced with non-functional scar tissue, which stiffens the heart wall and leads to chronic heart failure. While therapies have been investigated, cell-based therapies have failed to resolve this issue, as transplanted cells do not survive or engraft effectively in the injured tissue.
A new study in Advanced Science details a new, promising strategy: Preconditioning human adipose-derived stromal cells (hADCs) with therapeutic red light before culturing them as 3D spheroids to improve their survivability and therapeutic potential. They call these angiogenesis-preconditioned spheroids (APCS)
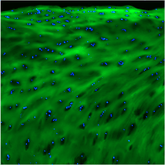
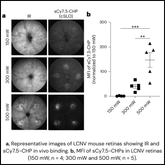
To precisely measure the therapy’s impact on tissue quality, researchers utilized our Collagen Hybridizing Peptides (CHPs). Unlike standard histological stains which only quantify the total amount of collagen, CHPs specifically bind to denatured collagen molecules - the molecular hallmark of active fibrosis - meaning CHPs provide a direct, quantifiable readout of fibrotic activity.
Continue Reading
In a rat model, hearts treated with red-light preconditioned spheroids showed significantly improved cardiac function. Critically, tissue analysis revealed significantly less CHP binding in the treatment group compared to all control and other treatment groups. Collagen Hybridizing Peptides provided the direct link researchers needed: The functional recovery they hypothesized was driven by an improvement to the heart’s molecular architecture. CHPs provided visual proof that their therapy prevented the accumulation of stiff scar tissue, which facilitated a higher quality of tissue repair.
This research established that red-light preconditioning of hASDC spheroids is a superior therapeutic strategy over currently available options for cardiac repair. The use of CHPs was essential to their conclusion, helping researchers move beyond functional metrics to provide direct, molecular-level evidence of reduced extracellular matrix damage. This confirms their therapy promotes a healthier myocardium by improving the quality of ECM.
The ability of CHPs to precisely quantify tissue quality is a critical tool for any lab looking to validate therapeutic efficacy and accelerate the development of anti-fibrotic or regenerative therapies facilitating true molecular repair