Pinpointing Fibrosis: How Collagen Hybridizing Peptides Illustrate Muscle Wasting in Pancreatic Cancer
Muscle wasting in cancer is estimated to contribute to approximately 30% of cancer-related deaths, with a deterioration of respiratory muscles implicated as a major cause of mortality. One of the most lethal cancers, Pancreatic ductal adenocarcinoma (PDAC), also has the highest prevalence and earliest onset of cachexia of all cancers. While researchers knew that inflammation and fibrotic scarring in the diaphragm are key drivers of cachexia, the timing and speed of the fibrotic progression was largely unknown. A recent paper in The Journal of Cachexia, Sarcopenia and Muscle sought to uncover the timing and mechanisms driving respiratory muscle wasting.
In order to monitor fibrotic remodeling in real time, the team couldn’t use standard histological collagen stains such as Picrosirius Red (PSR). These stains measure total collagen, giving a picture of collagen accumulation and fibrotic scarring after it occurs. The authors needed a solution to monitor fibrotic remodeling in real time. To show this, the authors used our Collagen Hybridizing Peptides (CHPs). Unlike tools that show the buildup of scar tissue, our CHPs provide a dynamic, real-time look at fibrotic remodeling by specifically binding to damaged collagen molecules.
The authors of this study injected murine pancreatic cells (KPC) orthotopically into mice and measured both total and damaged collagen in the diaphragm 1-2 weeks after injection. They found an increase in collagen and extracellular matrix proteins in general as cancer progressed, measured by PSR and Wheat Germ Agglutinin (WGA), respectively. They then stained with CHPs and found that on day 12, the time of cachexia onset, binding of CHP had doubled.
Continue Reading
CHPs show a unique utility compared to PSR in this example, as CHPs can illustrate active fibrotic remodeling, while PSR only shows accumulation of scar tissue as scarring occurs. CHPs allowed the researchers to pinpoint when remodeling is the highest and conclude that factors that degrade collagen are higher at the point of cachexia onset.
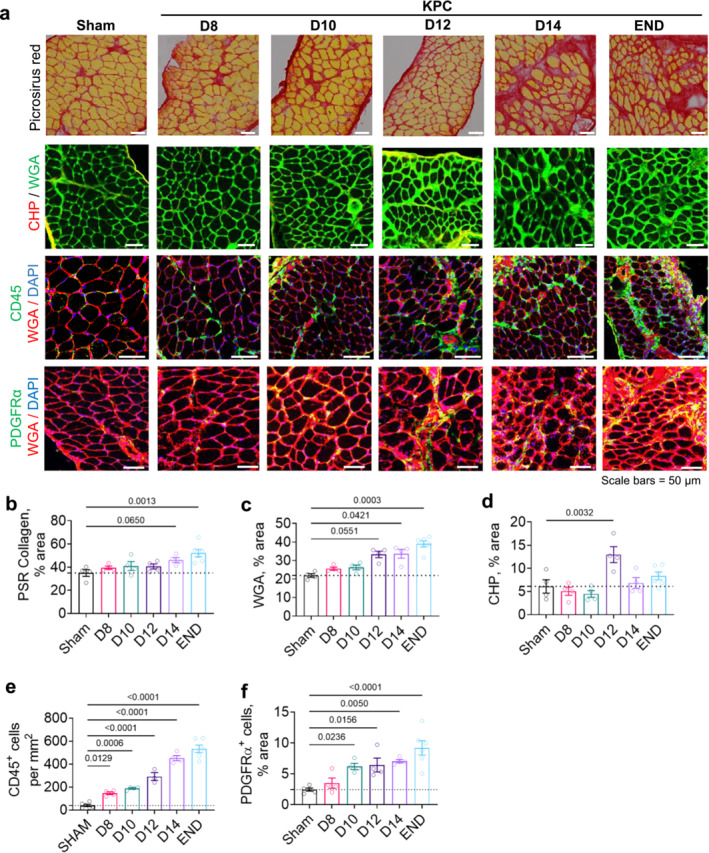
The ability of CHPs to quantify fibrotic remodeling and damaged collagen is clearly outlined in this example of PDAC. Using CHPs, the authors were able to pinpoint the exact timing of peak collagen degradation. CHPs allowed the question of when fibrosis is most active to be answered.
Discover how CHPs can allow for dynamic insight into fibrotic remodeling today.
FULL PAPER: Neyroud D. et al. Local Inflammation Precedes Diaphragm Wasting and Fibrotic Remodelling in a Mouse Model of Pancreatic Cancer. J Cachexia Sarcopenia Muscle. 2025 Feb;16(1):e13668. doi: 10.1002/jcsm.13668. PMID: 39810606; PMCID: PMC11733308.