Resolving fibrosis by stimulating HSC-dependent extracellular matrix degradation
Fibrosis is not just characterized by extracellular matrix (ECM) component deposition, but it’s better described as an imbalance between the production and breakdown of the ECM. Current treatments for fibrosis largely focus on stopping ECM production, but there is a significant, untapped potential in promoting its breakdown. Matrix metalloproteinases (MMPs) are enzymes that degrade collagen, a major component of the ECM and are key to breaking down ECM. While the role of other cell types like macrophages in collagen degradation has been studied, the contribution of hepatic stellate cells (HSCs), the primary cells responsible for depositing collagen in liver fibrosis, has been largely under-researched until now, with the groundbreaking study by Sharma et. al.
The researchers previously showed that inhibiting an enzyme called acid ceramidase (aCDase) increases ceramide levels in HSCs, which helps alleviate liver fibrosis in mouse models. In this new study, they aimed to understand the mechanism behind this. Using a combination of proteomics and RNA sequencing, they found that ceramide promotes a "collagen degradation" pathway in human HSCs. It does this by activating a specific signaling cascade: ceramide activates protein kinase Cα (PKCα), which then activates extracellular signal-regulated kinase 1/2 (ERK1/2). This, in turn, leads to the induction of matrix metalloproteinase 1 (MMP-1), a key collagen-degrading enzyme.
Continue Reading
To put this to the test in vivo, the researchers created mice where aCDase could be deleted in HSCs. When these mice were given CCl4, a chemical inducer that promotes lipid peroxidation and subsequent trigger of a local inflammatory response, they saw that deleting aCDase in their HSCs led to a significant increase in collagen degradation and a reduction in fibrosis. The researchers also developed a new, highly potent small-molecule aCDase inhibitor, which they found was effective in both halting the progression of fibrosis and promoting the regression of established fibrosis in two different mouse models.
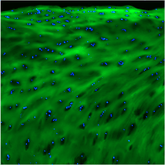
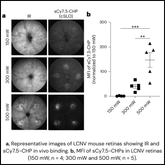
So, how did the scientists prove that collagen was actually being degraded? By staining liver tissue sections with collagen hybridizing peptides (CHPs), the researchers could visually confirm and quantify the breakdown of the collagen scaffold. This was used both to validate the researchers’ inducible aCDase deletion model as well as the efficacy and mechanism of their therapeutic molecule (“5A”). In the mice where aCDase was deleted in HSCs, the CHP signal was significantly increased compared to control mice. Even more compelling, this strong CHP signal overlapped with the fluorescence of the HSCs themselves, providing direct evidence that HSCs are indeed responsible for degrading the collagen matrix in the liver.

This finding was the "missing link" that connected the molecular signaling pathway with the functional outcome. It showed that inhibiting aCDase leads to increased collagenase activity in HSCs, which directly results in the breakdown of fibrotic tissue. CHPs were also able to fill the gap between a static and dynamic read-out—while Sirius red staining was able to show a reduction of bridging fibrosis following treatment, CHPs were actually able to show active degradation and removal of the collagen by HSCs.
This study is a game-changer for several reasons. First, it definitively establishes HSCs as key players in resolving liver fibrosis, not just causing it. Second, it reveals a clear, actionable therapeutic target: the aCDase-PKCα-ERK1/2-MMP-1 pathway. Finally, this work demonstrates the immense value of tools like CHPs. By providing a clear, quantifiable readout of collagen damage, CHPs allow researchers to directly link a molecular intervention (like inhibiting aCDase) to its functional effect on tissue architecture. This approach can be applied to many other research fields and disease states where ECM remodeling is a factor, from cancer to chronic wounds.