CD206+IL-4Rα+ Macrophages Are Drivers of Adverse Cardiac Remodeling in Ischemic Cardiomyopathy
Myocardial infarctions (MI), or more commonly known as heart attacks, have prolonged health implications that affect millions worldwide. Chronic heart failure (HF) is very common after a heart attack, with about 20-30% of patients developing it within a year. Heart failure after MI is characterized by distinct structural, cellular, and molecular changes that differentiate it from the healing phase. This includes adverse extracellular remodeling of the left ventricle (LV), characterized by LV chamber dilatation and fibrosis, as well as a distinct immune cell profile with a Th2/M2-like cytokine profile. Current research has heavily focused on the role of infiltrating monocytes in this process, but the contribution of resident macrophage populations—specifically how they sustain inflammation and promote scarring long after the initial injury—has remained unclear until the recent publication by Wang et al..
This group focused primarily on CD206+ macrophages, which are key mediators in the acute MI healing response, but have deleterious effects in the chronically failing heart. The researchers showed that the continued expansion of CD206+ macrophages in the chronic phase is a key driver of chronic heart failure. This macrophage subclass exhibit an M2-like phenotype, and it is known that activation with interleukin-4 (IL-4) can contribute to tissue fibrosis, driven by the secretion of FIZZ1 (found in Inflammatory Zone 1). FIZZ1 is a potent signal to cardiac mesenchymal cells, forcing them to differentiate into scar-forming myofibroblasts.
To test if this pathway could be interrupted, the researchers utilized advanced genetic models and antisense oligonucleotides. They found that deleting the Il4ra gene in myeloid cells halted the proliferation of these macrophages and stopped the progression of heart failure. Even more promising, they used Antisense Oligonucleotides (ASOs) to silence IL-4Ra in mice that already had established heart failure. This treatment effectively reversed left ventricular remodeling, improved heart function, and significantly reduced fibrosis.
Keep Reading!

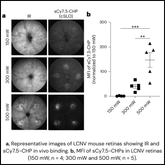
Figure 2B. 98% of the CD206+ macrophages were associated with the CHP-stained damaged collagen in the infarct and border regions.
However, the scientists were also interested in understanding the spatial distribution of these profibrotic macrophages. By using Collagen Hybridizing Peptides (CHPs), the researchers were able to visualize the specific microenvironments of active tissue remodeling. While analyzing total collagen accumulation is an important part of fibrosis, it only provides a static snapshot of the disease. CHPs solve this problem by highlighting where collagen is actively being remodeled or damaged, providing a more active picture of disease progression. In this study, CHPs provided critical spatial resolution that standard stains could not. The researchers discovered that CD206+ macrophages were not randomly distributed; they were almost exclusively clustered in CHP-positive regions. In the infarct and border zones of the failing heart, over 98% of these macrophages were physically associated with CHP signals. Furthermore, when the researchers injected these IL-4 polarized macrophages into healthy heart they saw an expansion of donor macrophages specifically at sites of CHP-identified collagen turnover, confirming these cells create a microenvironment of active injury.
This finding provided the crucial "spatial link" between the inflammatory cellular profile and the associated extracellular matrix damage. The extracellular matrix has long been regarded as an inert substrate; however, important research, such as this paper, reveals the inherent connection between immune cell populations and their extracellular environment. These alternatively activated macrophages onlnot just exist in the tissue but also actively congregate in areas of the most severe damage in the heart, where the extracellular matrix is being aggressively remodeled. This research suggests that ECM-targeted therapeutic strategies could have a unique advantage in treating chronic heart failure.
This study represents a significant advancement in cardiac research. First, it identifies the importance of CD206+IL-4Ralpha macrophages following MI, along with the importance of secreted proteins such as FIZZ1. Second, it offers a tangible therapeutic strategy by targeting IL-4 signaling. Ultimately, the study highlights the distinct advantages of CHPs. By identifying regions of active collagen turnover, CHPs allowed the researchers to map the precise spatial profile of the macrophages in relatively to the areas of highest collagen remodeling. This research supports the importance of understanding ECM biology in order to develop new treatments to solve chronic diseases like heart failure.