Beyond Scar Tissue: Can Understanding Cardiac ECM Remodeling Revolutionize Heart Repair?
Cardiovascular biology has seen significant advances in recent times, yet heart disease remains the leading cause of morbidity & mortality worldwide. A critical challenge following an acute Myocardial Infarction (MI, heart attack) is the irreversible loss of millions of cardiac muscle cells (Cardiomyocytes, CM). These lost cells are replaced by fibrotic scar tissue. While scarring is initially necessary to maintain rigid tissue structure immediately after injury, long-term presence of this non-functional tissue ultimately leads to heart failure.
This scarring represents a significant hurdle in Human MI. While research clearly shows lower vertebrates' ability to regenerate CM and resolve fibrosis, humans lack this capability. The fundamental difference between human biology and available animal models leaves researchers without adequate therapeutic strategies for MI in mammals.
There remains a pressing need to develop effective ways to replace and functionally regenerate lost heart tissue and to prevent scar-induced heart failure. Addressing this critical gap in understanding cardiac regeneration requires tools capable of providing insight into the complex tissue dynamics occurring at the injury site. The precision and selectivity of Collagen Hybridizing Peptides (F-CHP, 3Helix, Inc.) for damaged collagen molecules make them invaluable for pushing forward our understanding of MI.
Continue Reading
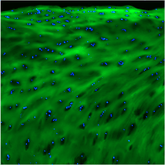
The ability to visualize and quantify the precise locations & extent of collagen degradation at the wound border was paramount. First, This paper hypothesized that proper extracellular matrix (ECM) dynamics at the injury border zone are essential for cardiomyocyte protrusion and invasion required for tissue repair. They also hypothesized that the ECM is disrupted in the absence of key cells like macrophages, preventing CM intrusion. Using CHPs, researchers showed a complete loss of collagen remodeling/degradation in absence of macrophages, establishing a direct link between macrophage presence & ECM remodeling, and how this prevents cardiac repair. In other words, CHPs provided the direct, quantitative evidence needed to unravel the complex ECM dynamics at play, revealing how crucial these processes are for effective treatment.
Collagen Hybridizing Peptide staining (blue) lost in the absence of resident macrophages, confirming their direct contribution to ECM remodeling, allowing CM infiltration & ultimately tissue regeneration."
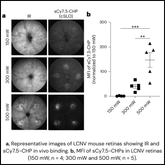
Furthermore, the research posed the question: what determines macrophage presence & activity? Knowing how to recruit and stimulate macrophage activity could be a promising therapeutic strategy. So, to answer this question, researchers investigated collagenase activity hypothesizing that macrophages will only be present and active while tissue is actively being broken down. First, researchers showed co-localization of CHPs and MMP14b to quantify collagenase activity. And, In line with their hypothesis, they observed mutant zebrafish lacking MMP14b to have significant decreases in both collagen breakdown and number of macrophages present when compared to their MMP14b+ counterparts.
Collagen Hybridizing Peptide staining (blue) co-localizes with collagenase (mmp14b) activity at the injury border zone, confirming its role in regulating the ECM post-MI
Collagen Hybridizing Peptide staining (blue) co-localizes with collagenase (mmp14b) activity at the injury border zone, confirming its role in regulating the ECM post-MI
The researchers’ newfound clarity profoundly impacts the broader landscape of MI research and future patient care. By precisely visualizing and quantifying collagen degradation & remodeling, and associating these processes with specific cell types, CHPs greatly expanded the researchers’ ability to investigate intricate ECM dynamics. These findings provide a new, crucial mechanistic foundation, illuminating new therapeutic targets in the development of pro-regenerative strategies aiming to functionally replace lost cardiac tissue. Ultimately, the enhanced understanding provided by tools like CHPs accelerates the journey toward innovative, patient-oriented solutions for a disease affecting millions globally.
Constanty, F., Wu, B., Wei, KH. et al. "Border-zone cardiomyocytes and macrophages regulate extracellular matrix remodeling to promote cardiomyocyte protrusion during cardiac regeneration" Nat Commun 16, 3823 (2025). https://doi.org/10.1038/s41467-025-59169-4