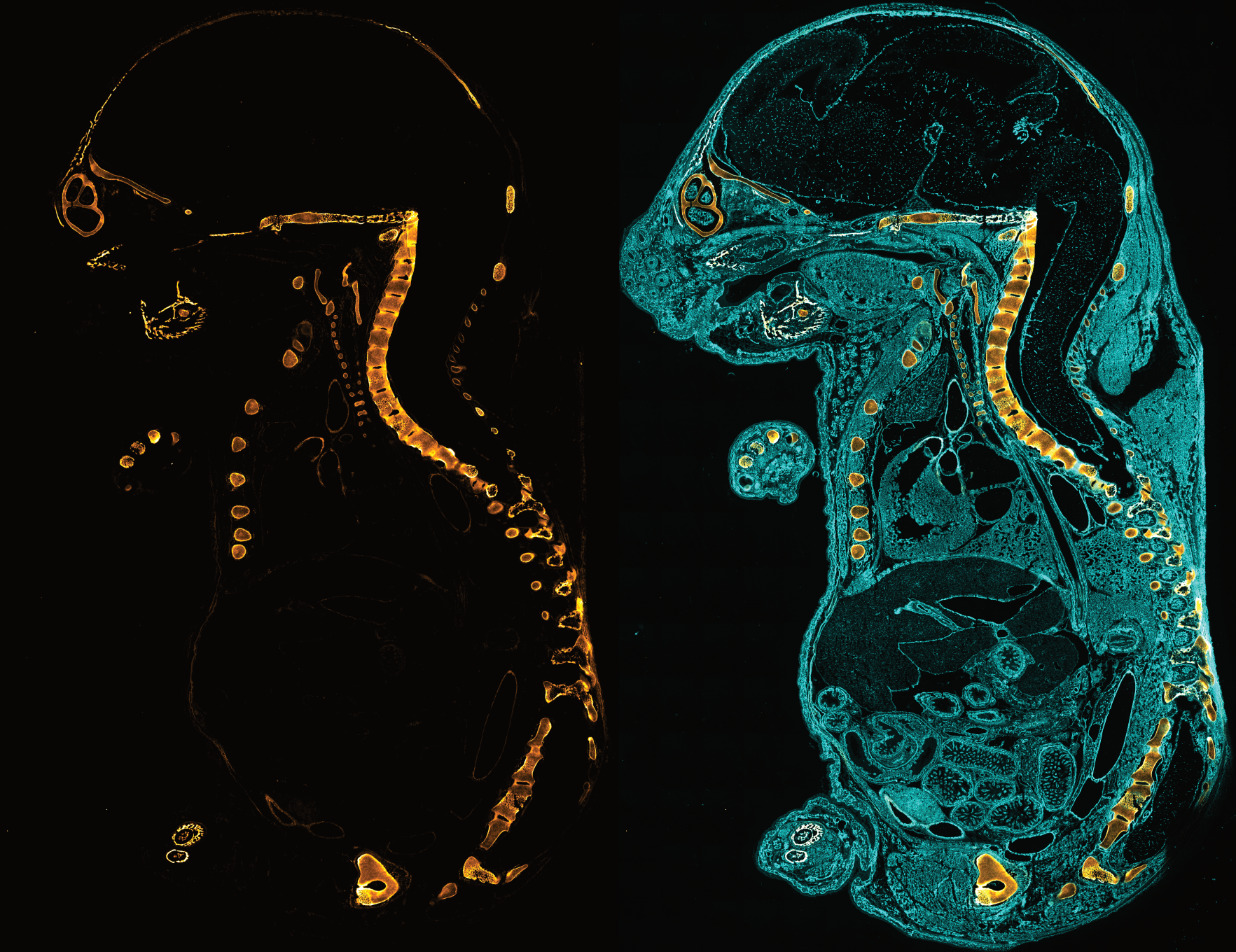
Collagen Hybridizing Peptides Suggest a Correlation Between Collagen Degradation in and Recruited Inflammatory Cells in MI
Introduction
Myocardial Infarction (MI) is a leading cause of death globally. MI occurs when blood flow to parts of the heart are blocked long enough to cause tissue damage and/or death. Accurate diagnosis and assessment of myocardial fibrosis post-heart attack is crucial for effectively managing the disease. Left unchecked, fibrotic remodeling of arterial ECM can lead to stiffened heart muscle, reducing cardiac output and increasing susceptibility to additional cardiac events. Where traditional methods fail to detect fibrotic changes, Collagen Hybridizing Peptides offer a clearer picture.
Citations
Neff, Lily S., et al. "Role of macrophages in regression of myocardial fibrosis following alleviation of left ventricular pressure overload." American Journal of Physiology-Heart and Circulatory Physiology 326.5 (2024): H1204-H1218.
Ho, Yen-Chun, et al. "PROX1 inhibits PDGF-B expression to prevent myxomatous degeneration of heart valves." Circulation Research 133.6 (2023): 463-480.
Angelini, Aude, et al. "Sex-specific phenotypes in the aging mouse heart and consequences for chronic fibrosis." American Journal of Physiology-Heart and Circulatory Physiology 323.2 (2022): H285-H300.
Widiapradja, Alexander, et al. "Replacement of lost substance P reduces fibrosis in the diabetic heart by preventing adverse fibroblast and macrophage phenotype changes." Cells 10.10 (2021): 2659.
Humeres, Claudio, et al. "Smad7 effects on TGF-β and ErbB2 restrain myofibroblast activation and protect from postinfarction heart failure." The Journal of Clinical Investigation 132.3 (2022).
Khalil, Hadi, et al. "Cell-specific ablation of Hsp47 defines the collagen-producing cells in the injured heart." JCI Insight 4.15 (2019).
- Choosing a selection results in a full page refresh.